National experts identify strengths, weaknesses, opportunities and threats to public health infrastructure
The pandemic has put the spotlight on public health – the workforce, infrastructure and underlying information systems designed to collect, analyze and manage public health data.
Informatics, medical information technology, and public health experts from across the country gathered at a symposium at the National College of Health Informatics said that how public health agencies receive and share information is “strategically designed, The information infrastructure for leveraging technology to deliver information is outdated.” To provide essential public health services on a daily basis and to respond effectively to public health emergencies. Their report explores the strengths, weaknesses, opportunities and threats posed by public health information systems.
Among the nine strengths included Yeoman services performed by public health workers and officials who worked on the system during the pandemic. A total of 22 weaknesses were detected. In addition, 14 opportunities and 14 threats were also identified.
“Pandemic experience has shown weaknesses in public health data systems and information technology. Many of them were developed before his 1990s and are obsolete,” said Brian E. Dixon, Ph.D., MPA of the Regent Reef Institute and Indiana University Fairbanks School. He is the Director of Public Health Informatics for Public Health, co-chair of the Symposium Planning Committee, and senior author of that report. “We found that we still used faxes to collect, share and manage information. Hospitals, laboratories and others were faxing data to public health departments. , requires a human to re-enter another system, which is completely inefficient.
“Nowhere is public health more integrated than, say, the banking system in this country. Sending information in is more difficult than transferring money into the financial system.”
Dr. Dixon said the 2009 Act, “HITECH,” which stands for Health Information Technology for Economic and Clinical Health, provided more than $30 billion in investments for healthcare systems to support the adoption of electronic health records. However, it points out that no investment has been made in the public health sector. . This kind of investment will bring about a similar transformation, helping the United States better prepare for the next pandemic, or even the next measles outbreak in certain states.
he said: “It’s not that simple to program a computer to do something. We have to develop the system in a way that makes it easier for humans to do the work. The goal of public health is to find out where the disease is in the community.” and strive to make communities healthier and prevent disease, but also connect people to care so that they get care when they need it.
“As the pandemic subsides, we are now at a point where we can reflect. We can look back over the past few years and see what worked and what didn’t. We can learn from it and apply that knowledge to recommendations on how to prepare, update and extend our systems for the future.”
Additionally, Dr. Dixon points out that many state and local health departments have systems that collect information from various sources such as hospitals, clinics, laboratories, the public, and even restaurants. The system collects data on sexually transmitted diseases, communicable diseases, chronic diseases, injuries to emergency room visitors, and food poisoning. All these systems live in silos and are disconnected. These systems will have to be interactive, flexible, scalable, data-driven and updated to support mobile applications, he said.
In their symposium report, the experts present three actionable factors for building strengths and opportunities while addressing weaknesses and threats.
- addressing sustainable financing needs,
- Leveraging existing infrastructure and processes for information exchange and systems development that meet public health goals,
- Prepare public health workers to benefit from available resources.
“Strengths, Weaknesses, Opportunities, and Threats to National Public Health Information Systems Infrastructure: Synthesis of Discussions from the 2022 ACMI Symposiumwas published in JAMIA.
author:
Jessica C. Acharya1Catherine Stayes2, 3Katie S. Allen4,5Joel Hartsell3,6Teresa A. Cullen5,7Leslie Rennert8,9Donald W. Rucker10, 11Harold P. Lehman12Brian E. Dixon4,5
Affiliation
1Health Policy and Management, Informatics, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA.
2University of Utah College of Nursing, Salt Lake City, Utah, USA.
3University of Utah School of Medicine, Salt Lake City, Utah, USA.
FourIUPUI, Indianapolis, Indiana, USA, Richard M. Fairbanks School of Public Health, College of Health Policy and Management.
FiveCenter for Biomedical Informatics, Regenstrief Institute, Inc., Indianapolis, Indiana, USA.
6Epi-Vant, LLC., Salt Lake City, Utah, USA.
7Pima County Public Health Department, Tucson, Arizona, USA.
8School of Medicine, Medical College of South Carolina, Charleston, South Carolina, USA.
9South Carolina Health Sciences, Charleston, South Carolina, USA.
Ten1upHealth, Boston, MA, USA.
11Department of Emergency Medicine, Ohio State University, Columbus, Ohio, USA.
12School of Medicine, Johns Hopkins Medical School, Baltimore, Maryland, USA.
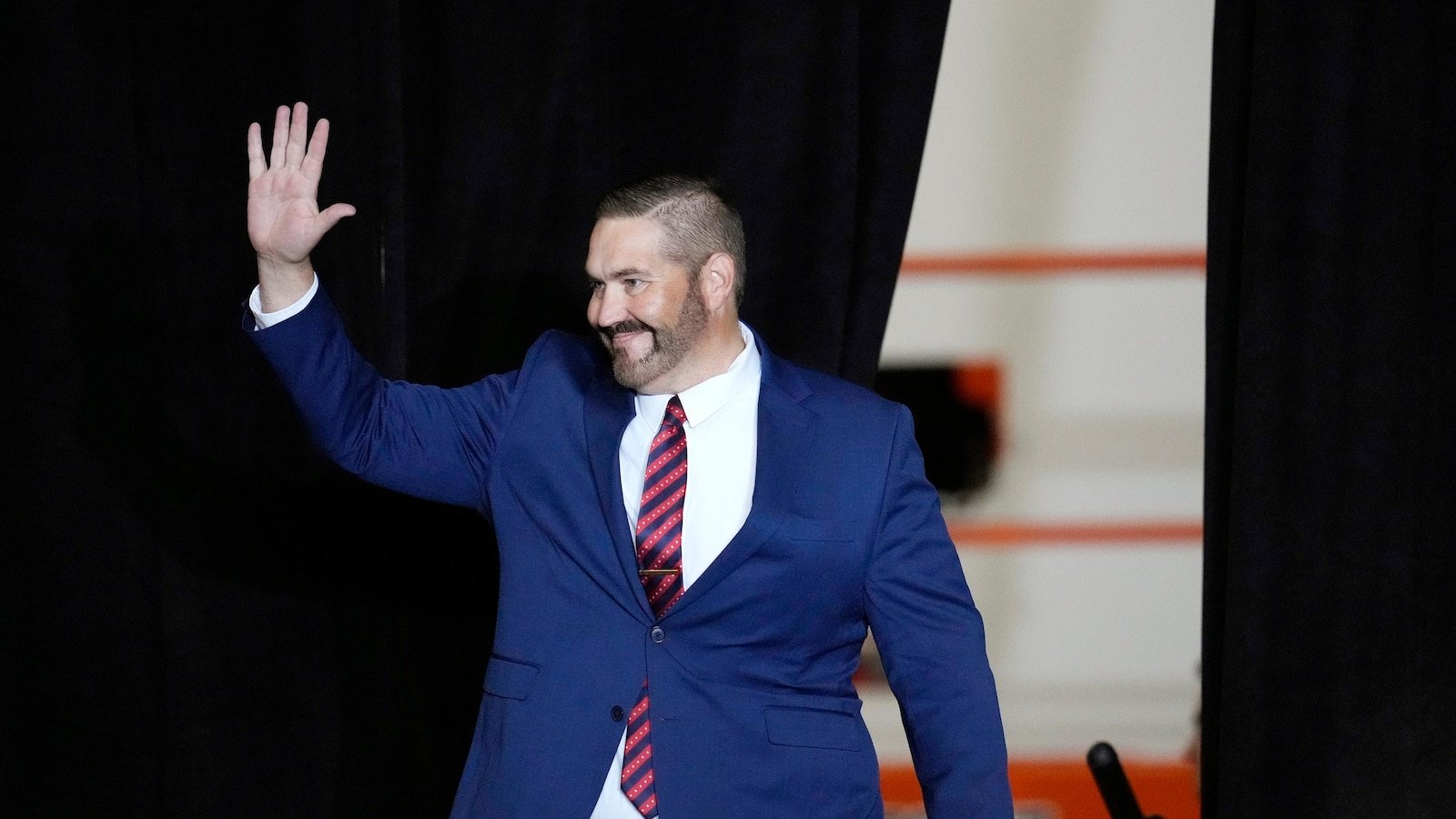
Dr. Brian E. Dixon, About MPA
Brian E. Dixon, Ph.D., in his role as interim director of the Clem Macdonald Center for Biomedical Informatics at the Regenstrief Institute and director of public health informatics at the Regenstrief Institute and the Richard M. Fairbanks School of Public Health at Indiana University. Additionally, MPA’s Brian E. Dixon, Ph.D. He is Professor of Epidemiology at the Fairbanks School of Public Health. He is also an Associate Investigator at the US Department of Veterans Affairs Medical Services Research and Development Center, Richard L. Ruudbusch VA Medical Center, and Research and Development Center for Health Information and Communications.
About the Regenströf Institute
Founded in Indianapolis in 1969, the Regenstrief Institute is a local, national and global leader dedicated to enabling a better informed world where people can fight disease and achieve true health. A principal research partner at Indiana University, Regenstrief and his research scientists are responsible for a growing number of major medical innovations and research. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic medical records, to improving patient-physician communication, to informing practice and improving the lives of patients around the world. It can range from creating models of improved care.
Sam Regenstrief, a nationally successful entrepreneur from Connorsville, Indiana, founded the institute with the goal of making health care more efficient and accessible to all. His vision continues to guide the Institute’s research mission.
About IU Richard M. Fairbanks School of Public Health
Located on the IUPUI and Fort Wayne campuses, the IU Richard M. Fairbanks School of Public Health is committed to improving public health and well-being through education, innovation and leadership. The Fairbanks School of Public Health is known for its expertise in biostatistics, epidemiology, cancer research, community health, environmental public health, global health, health policy and health services management.